First-in-class
First-in-class HDACi with disease-modifying potential for PAH
CS1 is our lead drug candidate currently in Phase II development, being advanced as a first-in-class treatment for the rare disease pulmonary arterial hypertension (PAH). CS1 is a histone deacetylase inhibitor (HDACi) that works through epigenetic modulation, uniquely targeting the underlying mechanisms driving disease progression in PAH.
In a completed Phase IIa trial, CS1 demonstrated a favorable safety and tolerability profile and showed data supportive of disease-modifying potential. The combined preclinical and clinical evidence is consistent with CS1 reversing pathological vascular remodeling, which is a core feature of PAH progression.
Importantly, CS1 is designed to be used on top of the current standard therapy for PAH, offering an additive disease-modifying benefit without compromising existing treatments.
Target
Targeting the underlying pathophysiology of PAH
CS1 is a novel, oral, controlled-release formulation of the Class I HDACi valproic acid (VPA). By targeting key disease-driving processes such as pathological vascular remodeling, CS1 has the potential to be an effective disease-modifying therapy for PAH patients also due to the favorable safety and tolerability profile. Furthermore, CS1 may be an effective treatment option providing an alternative that may alleviate patients from side effects affecting their everyday life.
In preclinical cardiovascular disease models, VPA has shown potential disease-modifying effects. including reverse pathological remodeling, as well as anti-fibrotic, anti-inflammatory, pulmonary pressure-reducing, anti-proliferative and anti-thrombotic effects.
The main objectives of the CS1 treatment are to enhance quality of life and extend life for patients with PAH. CS1’s unique efficacy profile aligns closely with the underlying mechanisms that drives the progression of PAH. This further position CS1 as a uniquely differentiated and highly promising treatment option.
The disease-modifying effects of CS1 has the potential to stop, halt or reverse the PAH disease progression
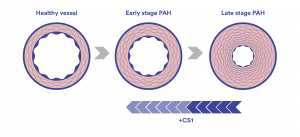
PAH is characterized by thickening and narrowing of the small arteries in the lungs, including the development of characteristic plexiform lesions, which restrict blood flow from the right side of the heart to the lungs. Over time, these changes, combined with increased tissue scarring (fibrosis), reduce the elasticity of the blood vessels and increase resistance to blood flow. This process, known as vascular remodeling, raises the pressure in the pulmonary arteries and impairs circulation. Epigenetic modulation through the effect of HDAC inhibition with CS1 has the potential to reverse the disease progression by reverse vascular remodeling.
IPR
Strengthened protection in patents and orphan designations
CS1 has a comprehensive patent portfolio comprising three patent families in key global markets. The development of CS1 in PAH is further supported by Orphan Drug Designation (ODD) from the U.S. Food and Drug Administration (FDA), granted in March 2020, and Orphan Medicinal Product Designation (OMPD) from the European Commission (based on EMA's recommendation) in August 2024. These designations recognize CS1's potential therapeutic benefit for a rare, life-threatening disease and confer important regulatory and commercial advantages, including:
- 7 years of market exclusivity post-approval in the US
- 10 years of market exclusivity in the EU
- Assistance with regulatory processes and potential financial incentives
Phase IIa
CS1 Phase IIa trial in PAH
A Phase IIa trial evaluating the safety, tolerability pharmacokinetics, and exploratory efficacy of CS1 on top of standard therapy in patients with PAH was completed in 2024. The Phase IIa trial was conducted at 10 US clinics over 12 weeks with a total of 25 patients of which 21 were evaluated for efficacy parameters. The trial successfully met its primary endpoint of safety and tolerability, with no drug-related serious adverse events.
The exploratory Phase IIa trial of CS1 identified efficacy signals suggesting reversal of pathological remodeling of pulmonary vessels. This was observed through:
- Signals of improved right ventricular function, which is the most significant predictor of mortality in PAH was observed through improvement of right ventricular global longitudinal strain (RV GLS) and reduced tricuspid regurgitation (TR)
- Signals of improved overall cardiac function was observed through improved NYHA/WHO functional class and Quality of Life (QoL)
- Signals of disease modification and prognosis was observed through improved REVEAL 2.0 risk score
Fast Track
Fast Track designation for CS1 in PAH
CS1 has been granted Fast Track designation by the FDA. The Fast Track designation enables closer and more frequent interaction with the FDA, eligibility for rolling review of submissions, and potential priority review. These advantages can help shorten timelines and strengthen the development pathway for CS1. For patients, it means that promising new therapies may become accessible more quickly.
EAP
Expanded Access Program for CS1 in PAH
CS1 has been approved by the FDA for an Expanded Access Program (EAP) as an extension of the Phase IIa trial in PAH. This program allows eligible patients who have completed the Phase IIa trial to continue CS1 treatment. Under an FDA-approved protocol, the EAP enables Cereno to collect long-term safety and efficacy data on CS1 use in PAH patients. This initiative supports ongoing treatment while providing valuable data for regulatory discussions and planning future Phase IIb or pivotal Phase III trials. Data from a follow-up after 4-months showed that findings are consistent with the Phase IIa trial results. The program will run for 12 months.
Read our policy further down the page.
“Fluidda study"
“Fluidda study:” Impact of long-term CS1 use on structural vascular changes
A sub-study of the EAP was initiated in February 2025 supporting the translation of the well-documented reverse vascular remodeling effects of CS1 in preclinical models to clinical practice. The lack of non-invasive methods available to demonstrate this effect in patients present a challenge. The innovative imaging technology Functional Respiratory Imaging (FRI), developed by Fluidda, has been explored as a non-invasive tool to solve this challenge by providing detailed, patient-specific insights into pulmonary vascular changes. The study is designed to include three CT scans in certain patients enrolled in the EAP during a 12-month period.
The study is expected to provide a visualization of how long-term treatment of CS1 on top of standard therapy may impact disease characteristic structural changes in small pulmonary arteries, demonstrated by improvements in blood vessel volume in these arteries on the CT images. This may provide valuable insights into CS1's disease-modifying potential that can transform the PAH treatment landscape.
Next steps
Preparations for further clinical development
The clinical development plan for CS1 is focused on continuing to evaluate it as a well-tolerated, orally administered therapy with a favorable safety profile and robust disease-modifying effects in PAH. Following the promising Phase IIa results, a larger, placebo-controlled Phase IIb trial is currently being planned. The FDA has endorsed the Phase IIb trial plans through a Type C meeting and a global top-tier CRO has been selected to lead the trial execution. The Phase IIb trial is anticipated to be initiated in H1 2026.
Updated August 2025.
Expanded access policy
At Cereno Scientific, our mission is to develop pioneering treatments to enhance and extend life for people living with rare cardiovascular and pulmonary diseases. We recognize the urgent needs faced by patients and their families, and we are committed to bring safer and more effective treatments to patients with high unmet needs.
We understand that there are times when an individual is unable to participate in a clinical trial, and other treatment options have been exhausted. In those cases, the individual's physician may choose to request access to an investigational drug outside of a clinical trial via what is often termed “Expanded Access” in the United States.
Expanded access, sometimes called “compassionate use” in the US, allows patients with serious or life-threatening conditions to gain access to investigational treatments outside of clinical trials, when no comparable alternatives exist. While participation in clinical trials remains the preferred path to access, we understand that this may not always be possible. If you are interested to learn more about expanded access, please visit the US FDA’s website.
Cereno Scientific currently has an ongoing Expanded Access Program that is for individual patients who have completed the CS1 Phase IIa trial in PAH (NCT06321705). If you fulfil this criterion and are interested in participation, please contact your treating physician for evaluation of eligibility.
Cereno Scientific does not have any other active Expanded Access Programs at this time.
In line with the 21st Century Cures Act, Cereno Scientific may revise this policy at any time.